Advanced filters
Blog
Our Chief Executive, Catherine Woodhead, has announced she will be leaving the charity this year.…
Blog
We’re delighted to announce, thanks to our partnership with LifeArc and the Lily Foundation, the…
Blog
We’ve been awarded the PIF TICK – the UK’s only assessed quality mark for print and online health…
Blog
A connection to nature
I’ve always felt connected to nature. Growing up in rural Lithuania, I was…
Your story
Over the past seven years as my limb girdle muscular dystrophy has progressed, I’ve become…
Your story
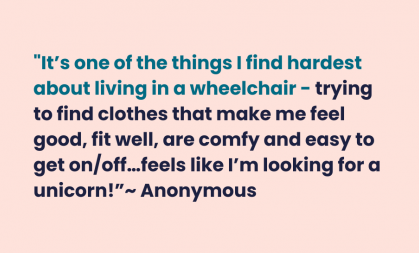
Thank you to everyone who responded to the survey about accessible clothing that I carried out last…
Blog
Thanks to my wheelchair accessible vehicle, I can travel far and wide, and since realising how good…
Blog
Several of my family members have Charcot-Marie Tooth (CMT) and have had to alter their life goals…
Blog
When I started university, I was studying Visual Communication. I created a Zine − a self-published…