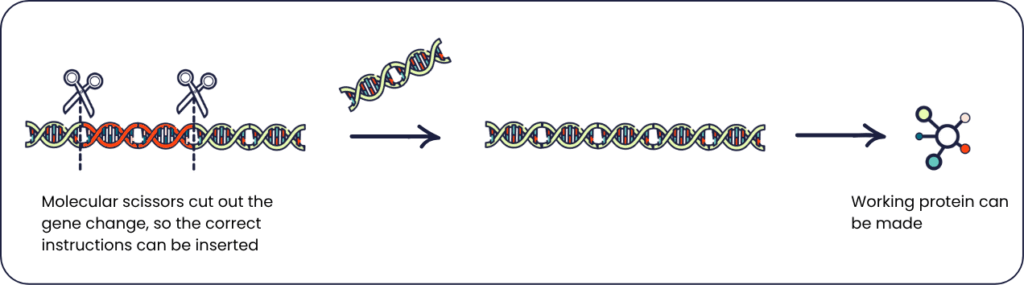
Researchers have found a way to repair one of the most common gene changes found in people living with limb girdle muscular dystrophy type 2B (LGMD2B). By using a tool called CRISPR, which acts like molecular scissors, they can cut out the gene change and replace it. In models that mimic LGMD2B, this approach allowed muscle cells to produce dysferlin, a protein essential for muscle repair and usually missing in this condition. While still in its early stages, this research could potentially lead to a treatment which helps damaged muscles repair and function properly again.
How gene editing could transform muscle repair

What is limb girdle muscular dystrophy?
Limb girdle muscular dystrophy (LGMD) is a group of conditions that generally cause weakness in the large muscles around the hips, thighs and upper arms. It’s caused by changes to genes – our body’s instruction manuals for making proteins needed to keep muscles healthy.
There are different types of LGMD, depending on which gene is affected. In LGMD type 2B (LGMD2B), the condition is caused by a change in the DYSF gene. This gene contains instructions for making dysferlin, a protein that plays an essential role in repairing muscles. When the gene is changed, dysferlin isn’t produced correctly. As a result, muscles can’t repair themselves properly and become gradually weaker and more damaged over time.
What is gene editing?
Gene editing is a technique used to correct gene changes. This can involve inserting, replacing, or removing parts of the gene’s instructions.
In this study, researchers used gene editing to replace the changed instructions in the DYSF gene with those found in people without LGMD2B. They used a tool called CRISPR, which acts like tiny molecular scissors, to cut out the change and insert the correct sequence, allowing the body to make working dysferlin.
Getting the treatment to the right place
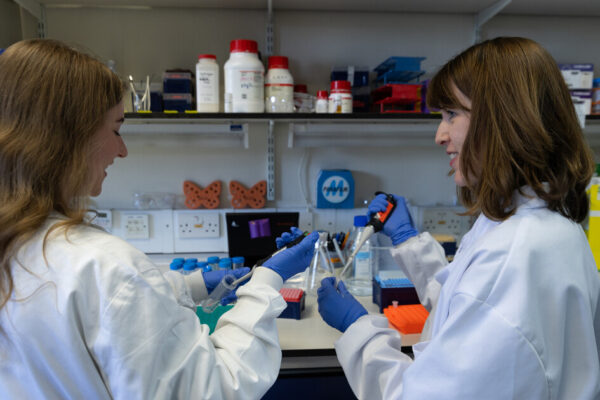
Our muscles go through a lot of wear and tear every day, which can lead to damage. Our bodies have special muscle stem cells, which help repair, grow and maintain healthy muscles. These stem cells can make copies of themselves and develop into different types of cells. When a muscle is damaged, the stem cells become activated and create new muscle cells to repair the damage and keep the muscle working.
In LGMD2B, genetic changes can be present in all cells, including muscle stem cells. So when stem cells create new muscle cells, the changes are passed on. This means the new muscle cells still don’t work properly, leading to ongoing muscle damage and weakening over time.
Researchers believe that targeting these muscle stem cells, using gene editing, could break this cycle. By correcting the changed gene in the stem cells, it may be possible to create muscle cells that can repair the muscle and help it function better. In theory, stem cells could be taken from specific muscles, treated in the lab, and then returned to the body to help restore muscle function.
Testing the treatment in models
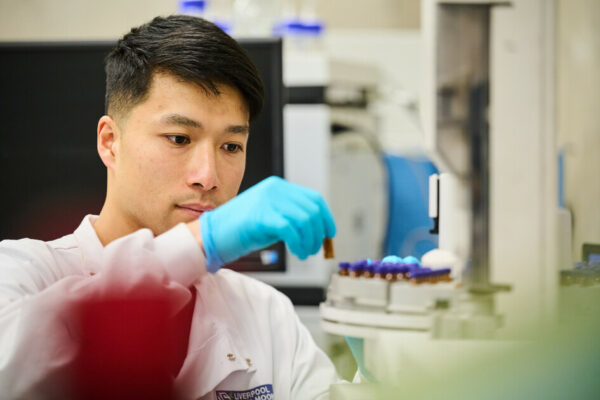
Before a potential treatment can be tested in people living with LGMD2B, it must first be checked to see if it is safe and has the potential to work. To do this, researchers use models that mimic the condition. This includes cells taken from people with LGMD2B or animals that have the same gene change and muscle repair issues.
In this study, researchers used muscle stem cells from two people with LGMD2B. After using the gene editing tool to correct the DYSF gene, the cells were able to produce working dysferlin. While encouraging, this didn’t yet show whether the corrected cells could help repair damaged muscles.
To explore this further, the team used a mouse model with the same DYSF gene change. They took muscle stem cells from the mouse’s leg, used the gene editing tool to replace the changed gene, and then transplanted the corrected cells back into the same muscle. After treatment, the cells produced working dysferlin, and the muscles began to repair and regrow.
Looking ahead
This early research shows that collecting muscle stem cells, correcting the gene change and returning them to the muscle may help muscles heal and work better. So far, this has only been successful in repairing a single muscle in a mouse. As the human body has over 600 muscles, it would be challenging to treat every affected muscle using this method. Instead, researchers think this approach could one day be used to target a few key muscles that are most impacted by LGMD2B – potentially improving strength and quality of life.
The research team is now working to move this approach towards clinical trials, where they can begin testing whether it works safely and effectively in people living with LGMD2B.