Pressure ulcers, also called pressure sores or bed sores, are injuries to the skin and the tissue below it. They happen when you stay in one position for too long without moving. This causes pressure on your skin and can reduce blood flow, which can damage the skin.
Understanding and preventing pressure ulcers
Pressure ulcers can also happen because of skin rubbing (friction) or skin layers sliding against each other (shearing), like when sliding down in a chair or bed.
Anyone can develop pressure ulcers, but some people are more likely to get them. This includes people who have trouble moving or need help to change position – like wheelchair users or people who spend a lot of time sitting or lying down.
With the right support and care, pressure ulcers can often be prevented.
It’s important to check your skin or your child’s regularly for changes. Pressure ulcers often start as a patch of skin that looks or feels different from the area around it. They can be painful and unpleasant.
Early warning signs to look out for:
- Patch of skin that looks red on white skin or purple or blue on black or brown skin. It does not change colour when pressed
- Skin that feels warmer or cooler than the area around it
- Change in texture – the skin may feel dry, flaky, hard or spongy
- Pain, tenderness, or itchiness in the affected area
- Swelling
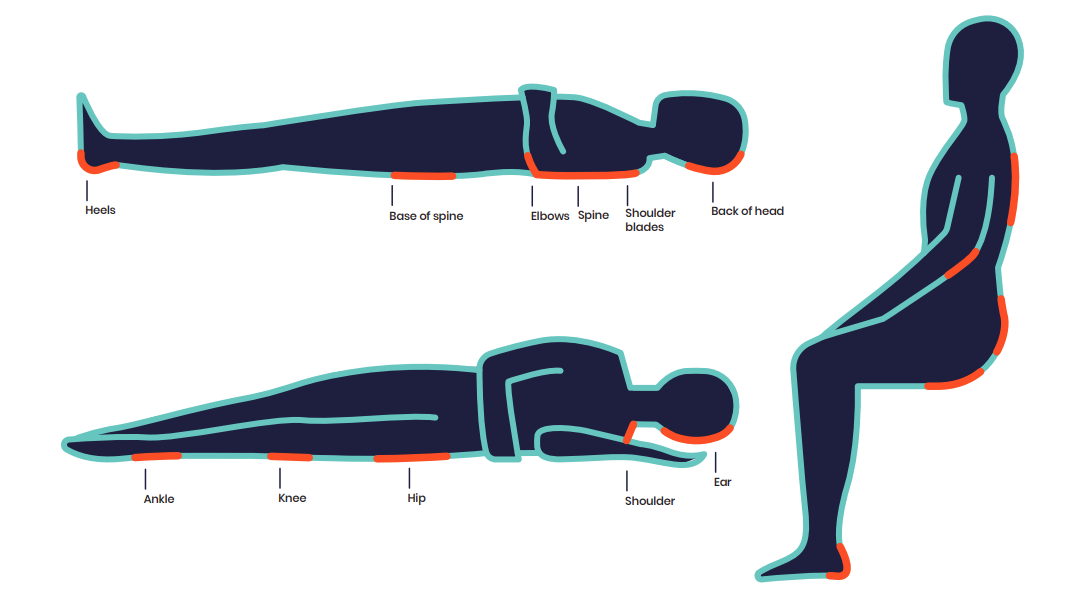
Where pressure ulcers can develop
Pressure ulcers can happen anywhere on the body. But they’re more likely to develop on areas where the bones are near the skin – like your elbows, shoulders, heels, hips, and bottom.
Pressure ulcers can also develop under devices and equipment that rest or press against your skin, such as splints, ventilation masks or glasses.
If you notice anything unusual, tell your GP or another healthcare professional right away. A pressure ulcer can get worse quickly if it’s not treated. It may become a blister or open wound. Getting help early can make a big difference and can help stop more serious damage or infection.
If you or your child are more likely to get pressure ulcers, there are simple things you, your family, or carers can do every day to help stop them from developing.
Depending on your needs, you might do these yourself or need some help:
- Change position regularly while in bed or sitting
- Use pressure-relieving equipment, like special cushions or mattresses if they’ve been recommended by your doctor
- Keep bedding and incontinence pads smooth – creases can press on the skin and cause damage
- Check skin every day for signs of redness, heat, or damage
- Keep skin clean and dry, and use moisturiser if it’s dry or flaky
- Eat well and drink plenty of fluids, as good nutrition helps keep your skin healthy
Getting help and support
It’s important to ask for help from your GP, occupational therapist (OT), community nurse, or other healthcare professionals if you’re worried about pressure ulcers. They can offer practical advice and help you get the right support.
Many hospitals have a Tissue Viability Service, run by nurses who specialise in skin and wound care. They can check the skin, give advice, and help with treatment. If you’re being cared for at home, you can get similar support from your local district or community nursing team. Your GP can refer you or your child to these services if needed.
If a pressure ulcer develops, treatment depends on how serious it is. The aim is to stop it getting worse, help it heal, and ease pain.
Treatment might include:
- Relieving pressure – by changing position and using pressure-relieving equipment
- Caring for the wound – to help the skin and underlying tissue heal, including cleaning and using dressings
- Caring for the surrounding skin – keeping it clean and dry, and protecting the area around the ulcer
- Managing pain – with medication if needed
- Treating infection – with antibiotics if the ulcer becomes infected
- Surgical intervention – complete removal of dead skin and covering with healthy tissue
Your healthcare team will work with you to make a treatment plan. Starting treatment early gives the best chance of healing.
Stopping pressure ulcers before they start can make a big difference. Following your care plan and looking after your skin every day can help stop them from coming back. If you ever have concerns, reach out to your healthcare team.
Author: Muscular Dystrophy UK
Reviewers: Sarah Jones, Maria Luvimin, and Dr Richa Kulshrestha
Last reviewed: June 2025
Next review due: June 2028
The information on this page was supported by AI and has been reviewed by specialists.
We’re here to support you
Webinars, Information Days, and support groups for our muscle wasting community. Our life-changing support is here for you.
Advice for living with or caring for someone with a muscle wasting condition.