The neuromuscular pathway outlines a comprehensive approach to adult care, covering diagnosis, management, and end-of-life support. It highlights barriers to effective care, recommends solutions, and sets key metrics to monitor and improve service delivery.
Developed by the Neurosciences Advisory Group (NNAG) with NHS England, the pathway supports local and national services in delivering high-quality care. It also helps identify gaps, ensure timely treatment, and address the needs of individuals with neuromuscular conditions.

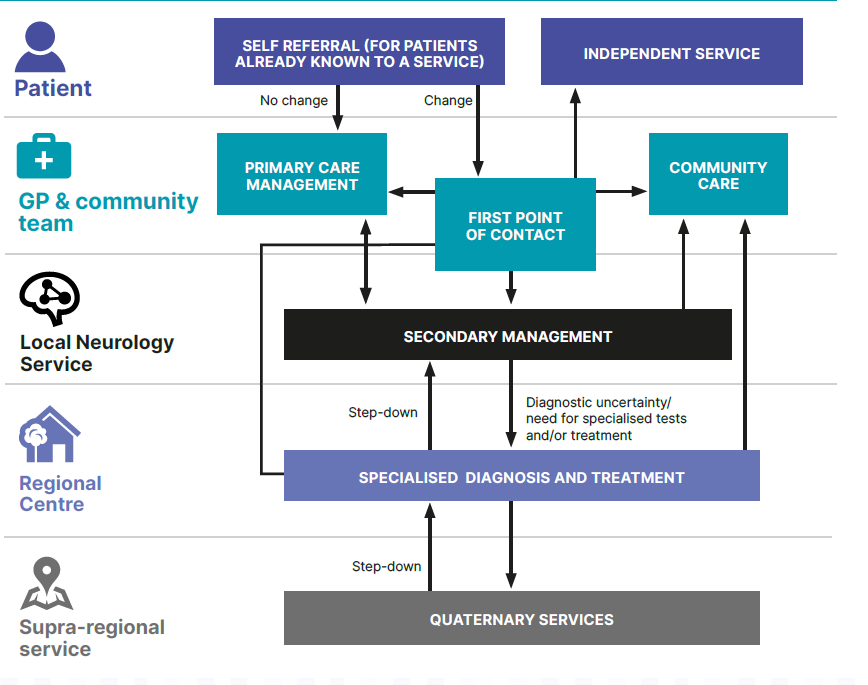
 Ideal practise
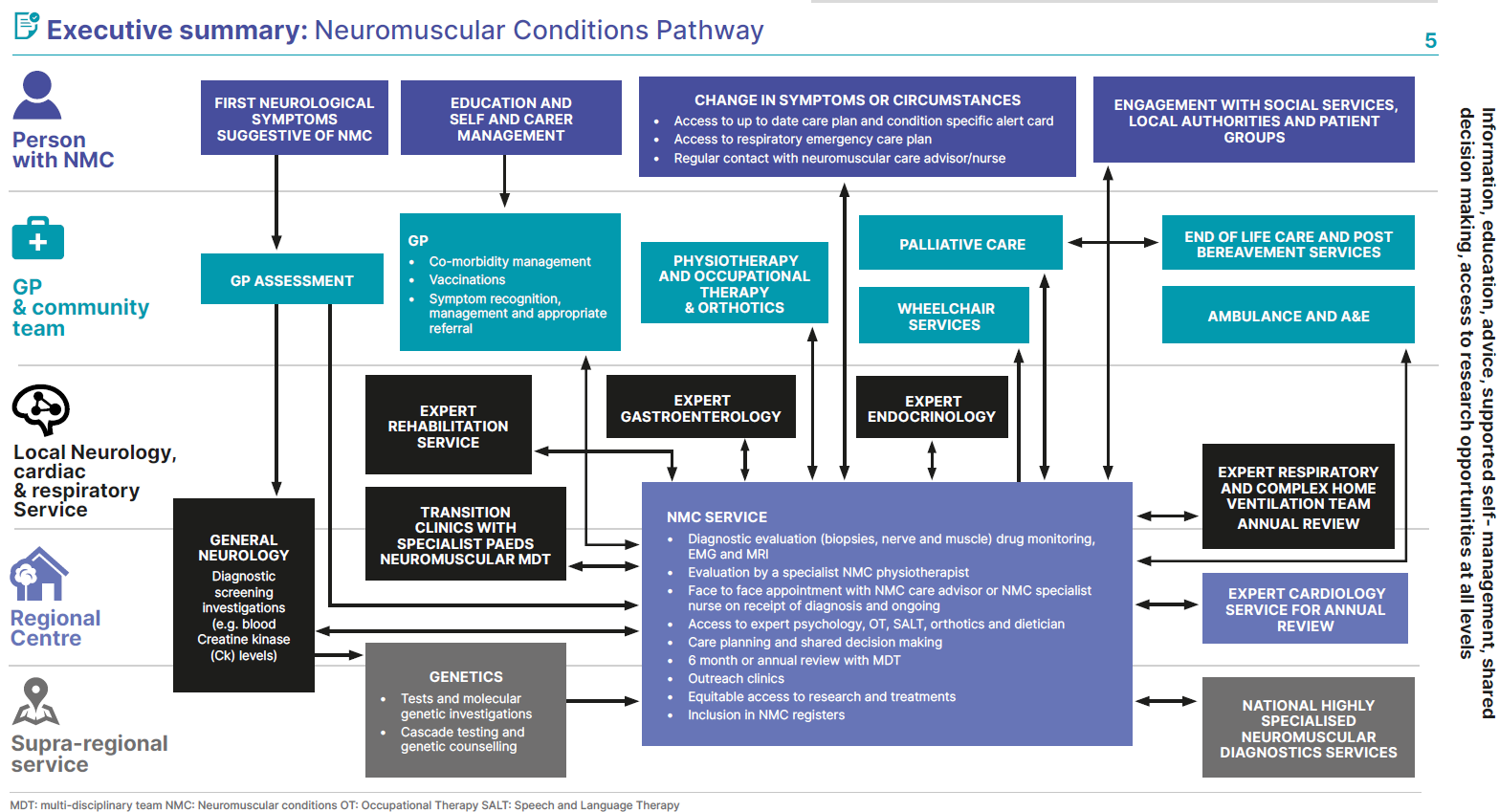
Ideal practise